Make a decision for your health now!
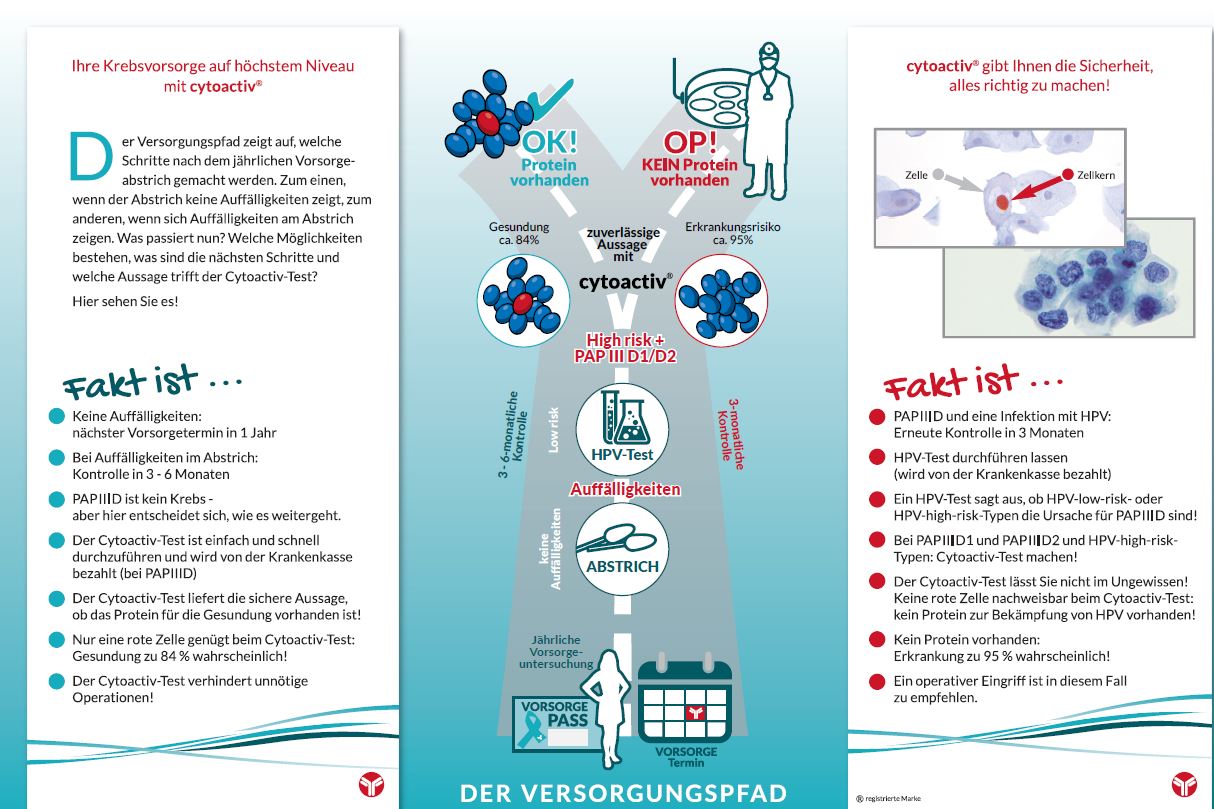
The care pathway shows what steps are taken after the annual screening smear. On the one hand, if the smear shows no abnormalities, on the other hand, if abnormalities appear on the smear. What happens now? What are the options, what are the next steps, and what does the Cytoactiv test tell us?
Find out and check out our flyer with the care path and lots of other important information!
By the way: You are welcome to request your personal preventive care passport from us. Send us a stamped, self-addressed envelope so that we can send you the screening passport free of charge.
Or ask your doctor about it.

Alle Infos
Nullam cursus
Vivamus aliquam
Nunc vitae erat
Proin posuere


Dr. Ulrich Mayer
Cytoimmun
ist perfekt

CHEFÄRZTIN
Maecenas eget molestie felis, sed facil
massa. Fusce cursus, mauris et ultri
dapibus, diam sem ulla mcorper

Franke Potente
750.000
MEHR ALS
FRAUEN JÄHRLICH IN DEUTSCHLAND
No more fear of dysplasia (PAPIIID) and cervical cancer (cervical carcinoma)
For many affected women, the gynecologist's control smear test as part of the annual cancer screening examination, called PAP smear test, is the beginning of a nightmare: The gynecologist informs the patient about an abnormal result and the mental carousel begins:
Is this a cancer diagnosis? Do I need a conization? How does this affect my desire to have children? Does this increase the risk of preterm birth? What does HPV infection mean for me and my partner? Have I been infected with high-risk group human papillomaviruses? What are HPV anyway?

We help you break out of this vicious circle!
Cytoimmun Diagnostics GmbH gives you the certainty with the cytoactiv® test whether your body has activated its self-healing powers. You get cancer care at the highest level. Don't give unnecessary, stressful and costly overtherapies a chance. If HPV is found, the cytoactiv® test can be used to determine whether the patient has developed a specific protein, L1, in her body.
If this "prognostic marker" - as it is called in technical jargon - is present, i.e. if the L1 capsid protein is detectable, the dysplasia is very likely to regress. However, the patient must know that spontaneous healing is not to be expected, usually the body needs up to 18 months to master this female disease.

EXCLUSIVE